Diabetes Mellitus subsequently refers to a group of common metabolic disorders that share the phenotype of hyperglycemia.
Moreover, It is one of the leading causes of end-stage renal disease with non-traumatic lower extremity amputations and cardiovascular diseases.
Additionally, It is one of the leading causes of morbidity and mortality in India.
Classification:
1.Type-1 Diabetes:
- It develops as a result of autoimmunity against the insulin-producing beta cells that result in complete or near-complete insulin deficiency.
2.Type-2 diabetes:
- It develops as a heterogeneous group of disorders characterized simultaneously by variable degrees of impaired insulin secretion, insulin resistance , and increased hepatic glucose production.
3. Specific types of Diabetes:
- A) Genetic defects or beta cell development
- B) Transient neonatal diabetes all in all
- C) Diseases indeed of exocrine pancreas-pancreatitis, pancreatectomy, neoplasia, cystic fibrosis, hemochromatosis
- D) Genetic defects simultaneously in insulin action, including type A insulin resistance, Lipodystrophy syndromes.
- E) Endocrinopathies- acromegaly, cushings’s syndrome, pheochromocytoma and hyperthyroidism.
- F) Infections also- congenital rubella, cytomegalovirus, coxsakievirus.
- G) Other genetic syndromes associated simultaneously with diabetes- Down’s syndrome, klinefeltor’s syndrome, turner’s syndrome and huntington’s syndrome.
- 4) Gestational diabetes mellitus.
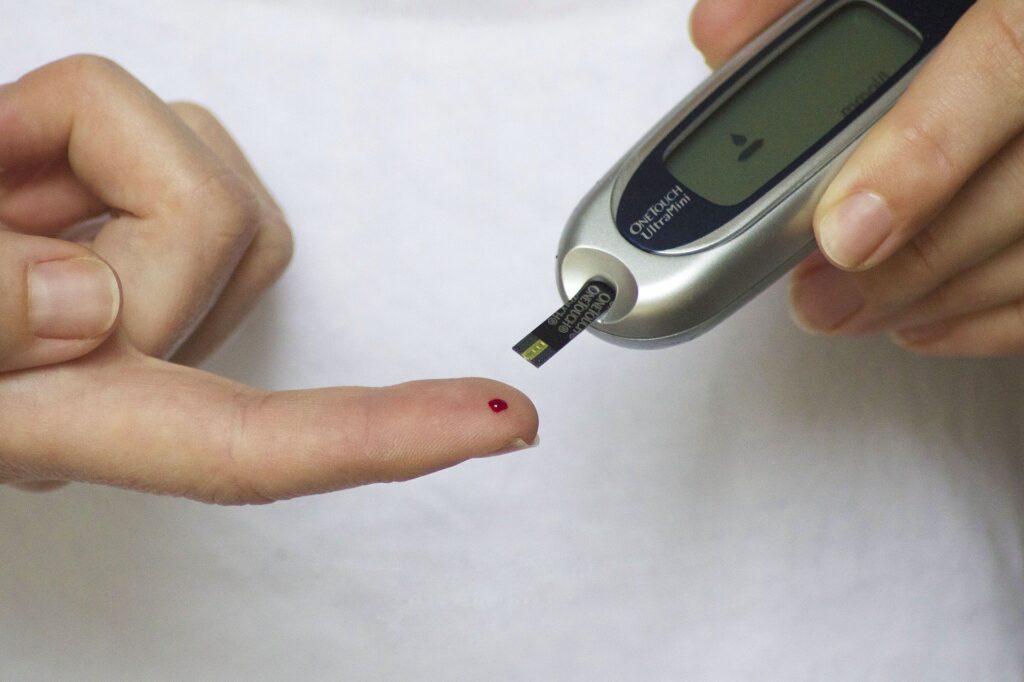
Criteria for diagnosis of diabetes mellitus:
- A) Symptoms subsequently of diabetes plus random blood concentration of >200 mg/dl
- B) Furthermore, Fasting plasma glucose > 126 mg/dl
- C)Additionally, HBA1c levels of >6.5%
- D) Moreover, 2 hours Plasma glucose levels of >200 mg/dl .
Screening :
- Use of HBA1C and FBS as a method of screening procedure is recommended because :
- A)Indeed, A large number of individuals who may have diabetes are asymptomatic and are unaware that they have the disease
- B) Studies have shown that the disease is present close to 10 years before diagnosis .
- C) Screening of diabetes of people ages >45 years is recommended every 3 years for early diagnosis and to start treatment initially to avoid any further complications .
Risk factors and signs for type-2 diabetes mellitus :
- A) Family history of diabetes (Parents or siblings with type-2 diabetes)
- B) Additionally, Overweight or Obesity related issues with BMI >25 kg/meter square
- C) Furthermore, Physical inactivity or sedentary lifestyle .
- D) Moreover, Race/ethnicity
- E) Previously identified with HBA1C OR IFG
- F) In addition, History of gestational diabetes mellitus
- G) Simultaneously, Hypertension or blood pressure of >140/80 mg/dl
- H) Moreover, HDL cholestrol levels of <35 mg/dl also
Pathogenesis:
A) Type-1 Diabetes Mellitus:
- It is defined as the immune mediated destruction of the pancreatic beta cells and insulin deficiency.
- Age-Most commonly seen before the age group of 20 years .
- In majority of patients simultaneously, autoantibodies act against the beta cell antigens which appear after this triggering effect, followed by progressive loss of insulin secretion.
- Additionally, when there’s decrease in the beta cell function varies depending on clinical diabetes and others developing the disease after couple of years.
- At autopsy, indeed many patients with long standing diabetes produce little amounts of insulin and some individuals with 50 years of the disease have insulin-positive cells in the pancreas.
- The major susceptibility gene for type-1 diabetes is located subsequently in HLA region on chromosome 6.
- The main immunological markers simultaneously involved with type-1 diabetes islet cell autoantibodies.
B) Type-2 Diabetes Mellitus :
- It develops as a result of insulin resistance , abnormal insulin secretion , increased hepatic glucose production , abnormal fat metabolism and systemic low-grade inflammation are the main centers for developing type 2 diabetes mellitus .
- Type-2 diabetes mellitus encompasses simultaneously a range of disorders with the common phenotype of hyperglycemia.
- Furthermore, It usually occurs at younger age groups and older age groups a lower BMI.
- Additionally, The most prominent genetic variant of transcription factor-7 gene 2 has been associated with type-2 diabetes mellitus.
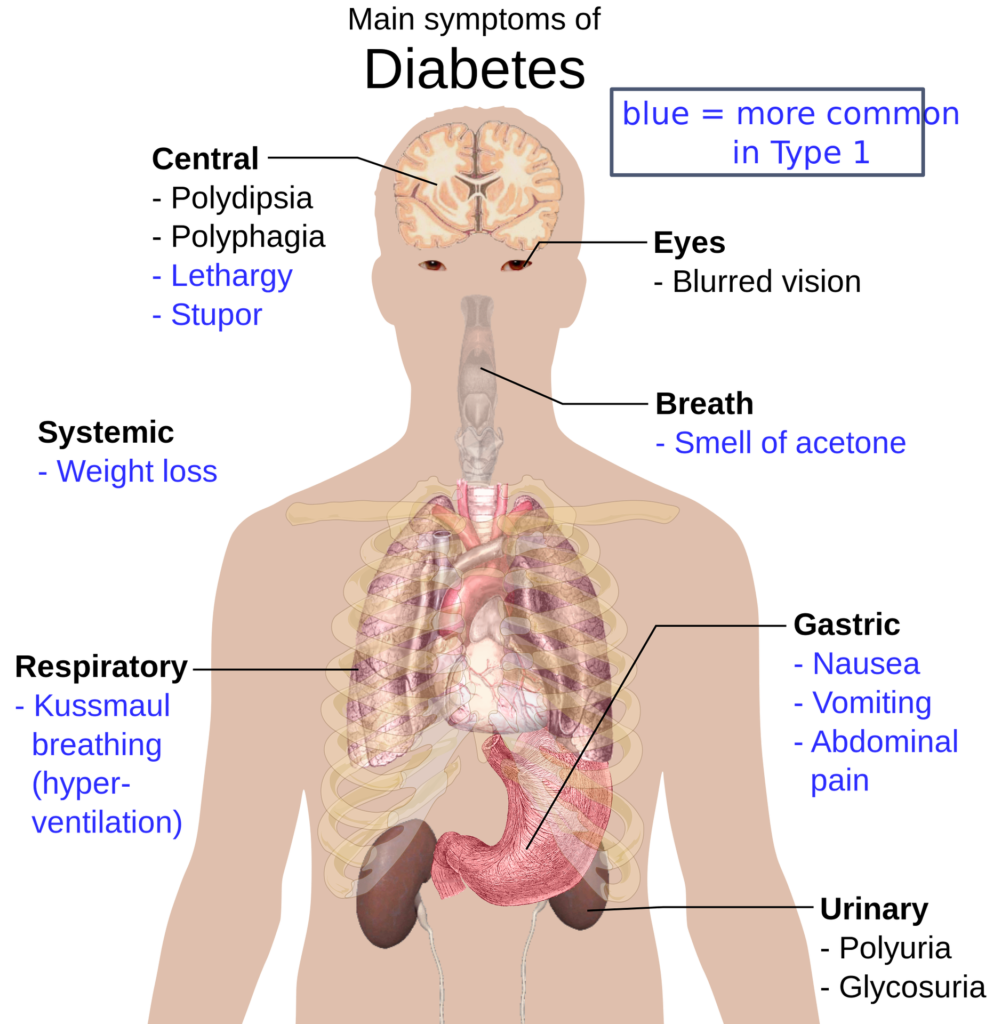
Approach to the patient with diabetes mellitus:
- Once the diagnosis is made for the cause of diabetes , emphasis on the symptoms related to diabetes ( acute or chronic ) and type of diabetes should be assessed .
A) History:
- Complete medical history should be assessed simultaneously with aspects involving weight , family history , sleep history , risk factors for cardiovascular diseases , history of pancreatic disease , and symptoms of hyperglycemia like polyuria , polydipsia , weight loss , fatigue , weakness , burry vision , and frequent superficial infections , and slow healing of skin lesions after minor trauma .
- Other initial factors simultaneously like previous HBA1C levels , self-monitoring of blood glucose levels frequency at which the patient has experienced hypoglycemia , complications and patients assessment about his knowledge on diabetes , exercise , nutrition and sleep history .
B) Physical examination:
- Additionally, Aspects like weight and BMI , retina examination , orthostatic blood pressure , foot examination , peripheral pulses and insulin injection sites .
- Annual foot examination should also be performed to assess blood flow , sensation , ability to sense touch , pinprick sensation , ankle reflexes , nail care , presence of foot deformities like charcot foot , claw toes and possible sites of ulceration on the foot .
C) Classification of diabetes mellitus in an individual patient:
- 1) Type-1 diabetes mellitus:
- Onset of disease present in less than 30 years age group
- Furthermore, Lean body habitus
- Additionally, Insulin therapy as initial therapy required
- Moreover, Ketoacidosis development
- Simultaneously, Autoimmune disorders like autoimmune thyroid disease , adrenal insufficiency , pernicious anemia , celiac disease and vitiligo.
- 2) Type-2 diabetes mellitus:
- In addition, Diabetic onset after the age of 30 years
- Furthermore, in obese patients
- Subsequently, Initial insulin therapy not required
- Simultaneously, Associated conditions like insulin resistance , hypertension , cardiovascular disease , dyslipidemia and polycystic ovarian syndrome .
D) Laboratory assessment:
- In addition, Serum insulin or C-peptide levels must be tested
- Furthermore, A low C-peptide levels in the setting of an increased blood glucose levels may confirm a patient’s need for insulin
- Moreover, Measurement of islet cell antibodies may be useful if the type of diabetes mellitus is not clear.
Treatment protocol :
| Mechanism of action | Examples | HBA1C reduction | Advantages | Disadvantages | Contraindication | |
| 1) Oral : | ||||||
| Biguanides | Decreased hepatic glucose production | Metformin | 1-2 % | Weight neutral , hypoglycemia avoided , Decreased CV events | Diarrhea , nausea , lactic acidosis , vitamin B12 deficiency | Renal insufficiency , CHF , Hospitalized patients |
| Alpha glucosidase inhibitors | Decreased GI glucose absorption | Voglibose , acarbose,miglitol | 0.5-0.8 % | Reduce post-prandial glycemia | GI flatulence, liver function test additionally | Renal/liver disease |
| Dipeptidyl peptidase IV inhibitors | Prolong endogenous GLP-1 action : Increased glucose , Decreased glucagon | Linagliptin , alogliptin , saxagliptin , sitagliptin | 0.5-0.8 % | Well tolerated , does not cause hypoglycemia | Angioedema | Reduced dose with renal disease |
| Sulfonylureas | Increased insulin secretion | Gliclazide , glimerpiride , glipizide , glibornuride | 1-2 % | Short onset of action , lower postprandial glucose | Hypoglycemia , weight gain | Renal/liver disease |
| Nonsulfonylureas | Increased insulin secretion | Mitiglinide , nateglinide | 0.5-1.0 % | Short onset of action , lower postprandial glucose | Hypoglycemia | Renal/liver disease |
| Sodium-glucose cotransporter 2 inhibitors | Increased renal glucose excretion | dapagliflozin , canaglifozin , ertugliflozin | 0.5-1.0 % | Decreased weight and BP , do not cause hypoglycemia | Urinary and genital infections , polyuria , dehydration | Moderate renal insufficiency |
| Thiazolidinediones | Decreased insulin resistance , increased glucose utilization | Pioglitazone , rosiglitazone | 0.5-1.4 % | Lower insulin requirements | Peripheral edema , CHF , weight gain , fractures , macular edema | CHF , liver diseases |
2) Parental:
| Amylin Agonist | Slow gastric emptying , Decreased glucagon | Pramlintide | 0.25-0.5% | Reduce postprandial glycemia, weight loss | Injection, nausea, increased risk of hypoglycemia simultaneously with insulin | Agents that slow GI motility |
| GLP-1 receptor agonist | Increased insulin, decreased glucagon, slow gastric emptying | dulaglutide, semaglutide | 0.5-0.99% | weight loss, does not cause hypoglycemia | injection nausea, increased risk of hypoglycemia | renal disease |
| Insulin | increase glucagon utilization, decreased hepatic glucose production | – | Not limited | known safety profile | injection, weight gain, hypoglycemia all in all | – |
Furthermore, Follow us for more such content here
Please refer this book additionally for detailed description of diseases: Harrisons book of internal medicine

