Critical care medicine-part 2 gives a brief description of how and why shock is an important factor to assess the condition of patients. For instance, Comprehensible care of critically ill patients who are deemed recoverable is carried out by skilled personal with life threatening or potential life threatening problems.
Shock:
- Definition-Clinical condition of organ dysfunction resulting from an imbalance between cellular oxygen supply
- And furthermore demand or presence of multisystem end-organ hypoperfusion.
- These conditions are commonly seen in Intensive care units (ICU).
- Subsequently, adequate oxygen supply can reverse the organ dysfunction in early shock.
- When its untreated the reversible process can turn into an irreversible phase leading to death from multisystem organ dysfunction.
- A thorough assessment simultaneously is required by the clinician for early intervention and to provide initial therapy to avoid irreversible organ multisystem dysfunction and death.
Initial evaluation( Critical care medicine-part 2):
- Clinical indicators include :
- a) Mean arterial pressure
- b) Tachycardia
- c) Tachypnea
- d) Cool skin,extremities
- e) Altered mental status
- f) Oliguria
- Initial evaluation of a hypotensive patient should also involve a thorough bed-side assessment of cardiac output.
Signs of decreased cardiac output in critical care medicine-part 2:
- 1) Narrow pulse pressure
- 2) Cold extremities with delay in the refill of capillary vessels.
Signs of increased cardiac output:
- 1) Widened pulse pressure
- 2) Warm extremities
- 3) Rapid capillary refill
- If a patient with “Hypotension shows signs of increased cardiac output”,then the reduced blood pressure is due to decreased systemic vascular resistance.
- The main cause of high cardiac output hypotension are as follows:
- a) Sepsis
- b) Liver failure
- c) Pancreatitis
- d) Burns
- e) Trauma
- f) Anaphylaxis
- g) Thyrotoxicosis
- h) Peripheral artriovenous shunts
- If a patient with “Hypotension shows signs of decreased cardiac output”,intravascular volume should be assessed based on the history that suggests hemorrhage or volume loss due to vomiting,diarrhea and polyuria.
- A) Reduced intravascular volume :
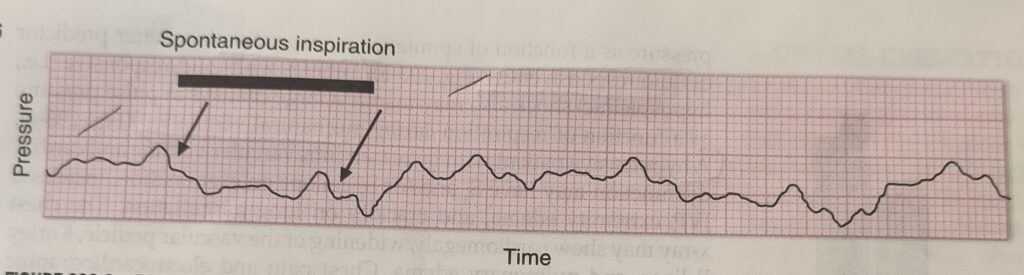
- (1) Any changes in the right atrial pressure with spontaneous respiration can predict the fluid responsiveness.
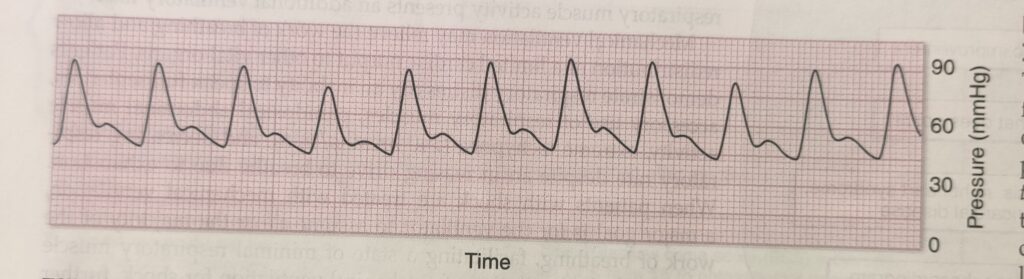
- (2)Patients with fluid responsive shock (hypovolemic) manifest with change in pulse pressure during mechanical ventilation.
- B) Increased intravascular volume and cardiac dysfunction(critical care medicine-part 2):
- On examination,shows S3 OR S4 gallop on ECG.
- Increased JVP
- Additionally, Edema
- Moreover, Crackles on lung auscultation.
- Chest x-ray shows cardiomegaly,widening of vascular pedicle,kerley B lines and pulmonary edema.
- Hence the most common types of shock are as follows:
- A) Hypovolemic shock
- B) Septic shock
- C)High output hypotension.
- On the whole,initial assessment of shock is vital for proper diagnosis with aggressive resuscitation being the intervention for survival from hypovolemic and cardiogenic shock.
- Ultrasound of thorax and abdomen is also done by intensivists for physical examination to assess volumes,adequacy of cardiac performances.
- In conclusion, The main goal is to reestablish tissue perfusion and to prevent end-organ damage with proper resuscitation.
Furthermore, For more content do visit here
Please refer this book simultaneously for detailed description of diseases: Harrisons book of internal medicine

